Immune diseases comprise a multitude of diseases such as chronic inflammatory bowel diseases, autoimmune diseases, multiple sclerosis and sarcoidosis, but also other diseases of different organ systems sharing the essential pathophysiological feature of a dysregulated immune system. The chronic inflammatory processes taking place in all these diseases damage affected organs, increase the risk of heart attacks, strokes and cancer and lead to reduced performance, fatigue and exhaustion. Immune diseases are therefore associated with significant limitations for patients. Approximately 8 percent of the world's population are affected. In the German-speaking world alone, more than 5 million people suffer from immune diseases.
Therapies so far have been based mostly on immunosuppression
Immune diseases so far have mostly been treated symptomatically with drugs unspecifically suppressing the patient's immune system. A causal and ideally individualized curative therapy is currently not possible. Due to the mostly chronic course, immune diseases are associated with considerable limitations for patients, who usually require a long-term immunosuppressive therapy. There is a great need for research both with regard to the pathophysiology and possible therapeutic target structures.
T-helper cells and their subtypes
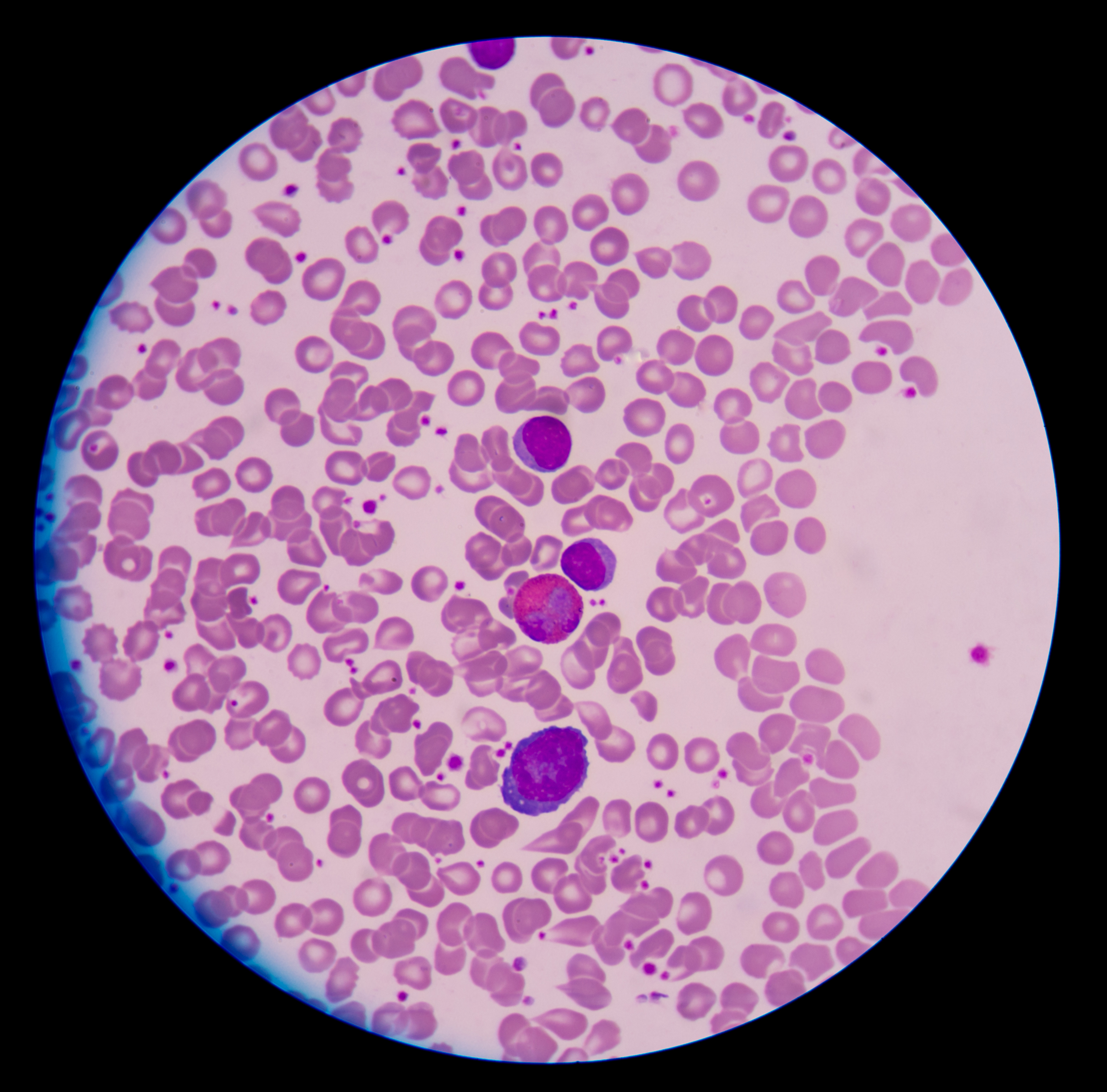
After antigen stimulation, naive T-helper cells (Th) differentiate context-dependently into different subtypes that trigger very different immune responses. Th1, Th2 and regulatory T-cells (Treg) have been known for a long time. Recently, new subtypes have been discovered, including Th17-cells.
Classical Th17-cells are now considered organ-protecting T-cells that promote tissue homeostasis, whereas Th17.1-cells have been described as highly pathogenic. Th17.1-cells produce proinflammatory cytokines and propagate autoimmunity. Especially for chronic inflammatory bowel diseases, autoimmune diseases, multiple sclerosis and sarcoidosis a central role of Th17.1-cells has been described. For all these diseases, there is a clinical need for new, targeted therapeutic strategies to replace the conventional immunosuppressive therapy with all its side effects. To date, there is no therapy specifically targeting Th17.1-cells. The Th17.1 immune response is increasingly emerging as a central pathomechanism of numerous chronic inflammatory diseases. Classical immunomodulators, such as corticosteroids, azathioprine, methotrexate, or cyclophosphamide have only a minor effect on the Th17 immune response which, moreover, is associated with considerable side effects. Although the new biologics can specifically switch off individual key cytokines of the Th17.1 immune response, this does not seem to convincingly curb the Th17.1 immune response effectively. Therefore, there is still a considerable clinical need for the development of new Th17.1 immune modulators.
 Fraunhofer Cluster of Excellence Immune-Mediated Diseases
Fraunhofer Cluster of Excellence Immune-Mediated Diseases